Brain Tumors
What Are Brain Tumors?
A tumor is a group of tissue within the body formed by abnormal cells. Brain tumors are the most common solid tumor found in the pediatric population. Each year, approximately 3,400 children are diagnosed with a primary tumor of the central nervous system (CNS)—comprising the brain and spinal cord.
Is it Brain Cancer? - Benign vs Malignant
While all primary brain tumors arise from cells originating in the brain, these CNS tumors can differ significantly with regards to location, cell origin and pathology, clinical manifestations, prognosis, and treatment options. Some of these tumors may exhibit a slow benign (noncancerous) growth pattern, while others are more aggressive and classified as malignant or cancerous. Due to the sensitive, important structures of the CNS, even a benign tumor may cause significant clinical symptoms if located in or near critical brain or spine structures. Similarly, surgical access to these so-called “benign” brain tumors can be limited or dangerous, making the tumor inoperable and thus the potential to act as a more malignant lesion over time.
Diagnosing a Brain Tumor
Advances in imaging with computed tomography (CT) and magnetic resolution imaging (MRI) allow clinicians to better visualize the mass and determine key characteristics that may help differentiate one tumor from another. By evaluating the tumor size and shape, identifying its location and effect on adjacent structures, and examining patterns of contrast enhancement (a substance that enhances the contrast of body structures on medical imaging), clinicians may be able to diagnose the tumor with imaging alone. Sometimes further studies, such as blood work or cerebrospinal fluid (CSF) analysis by lumbar puncture—also called a spinal tap—can also help with the diagnosis. When feasible, direct histological evaluation by either biopsy or tumor resection is the gold standard in diagnosing the specific tumor type. Often, however, the imaging, together with clinical presentation and a laboratory workup, can help clinicians formulate the best suitable treatment option for the patient.
Treatment of Brain Tumors
Treatment of brain tumors can vary widely and may include close clinical observation with interval imaging, surgical resection, chemotherapy, radiation, or a combination of these modalities. The exact combination of therapies will depend upon the expected behavior of the tumor, and clinicians will need to carefully weigh the risks and benefits of the treatments. Pediatric tumors and their treatment differ from their adult counterparts, especially as long-term effects from chemotherapy and radiation have a greater impact on the developing CNS of a child.
Brain Tumor Histology and Classification
There are more than 120 different classifications of tumors, most of which are classified by the cell type from which they arise. A better understanding of this classification system can be gained through a brief review of the cells that comprise the central nervous system and its coverings.
As a very general overview, the majority of CNS cells can be divided into two groups:
- neurons, which are cells that send and receive electrochemical stimulation to and from the brain and spinal cord
- and glial cells, the cells that support neurons.
Neurons
There are many different types of neurons found throughout the brain which carry a variety of signals depending on their function and location. Unlike many other cells in the body, neurons, do not regenerate after damage, although there have been notable exceptions to this rule.
Glial Cells
Glial cells are far more plentiful than neurons, making up about 90% of brain cells. These cells are further specialized to provide specific functions to support the neuronal tissue. Some glial cells function to provide structural or nutritional support, while others help to insulate the neurons, provide defense against pathogens, and clean up cellular debris. The most common glial cells are:
- astrocytes
- oligodendrocytes
- Schwann cells
- microglia
- ependymal cells
Covering the brain and spinal cord is a membrane called the meninges, comprised of meningothelial cells. Tumors may arise from any of these subtypes and thus be named according to their cells of origin. Hence, the terms astrocytoma, oligodendroglioma, ependymoma, etc. may sound familiar. You may frequently hear of tumors referred to as gliomas, or glial tumors. These are generally referring to tumors arising from astrocytes as these are most commonly the cell of origin.
The World Health Organization (WHO) has categorized gliomas into four classifications based on tumor aggressiveness and malignancy.
- WHO grade I tumors are low-grade lesions that are non-infiltrating and have well-defined borders. These tumors can be cured if in a location amenable to surgical resection. They are slow growing and may remain inactive, even if they are not completely excised. Examples of WHO grade I tumors include pilocytic astrocytomas and pleomorphic xanthoastrocytomas.
- WHO grade II tumors are more infiltrative. These tumors tend to invade normal tissue, making complete surgical resection more challenging than WHO grade I lesions, especially if the tumors are located in critical brain structures. These tumors tend to be slower growing than the higher-grade lesions, but they may evolve into WHO grade III or IV lesions over time. Examples of WHO grade II lesions are oligodendrogliomas and low-grade astrocytomas.
- WHO grade III tumors are known as anaplastic astrocytomas. They are considered malignant because they are infiltrating, fast growing, and often require treatment with surgical resection, chemotherapy, and radiation.
- Grade IV lesions, also known as glioblastoma multiforme (GBM), are even more aggressive than anaplastic astrocytomas and may grow so rapidly that they outgrow their blood supply and cause tumor necrosis. GBMs are malignant lesions with poor prognosis regardless of the treatment (e.g., surgery, radiation, and chemotherapy).
Embryonal Cell Tumors
Another cell type to note is the “embryonal” cell. In development, the neurons and glial cells are thought to derive from a common progenitor cell that differentiates at different stages depending on certain genetic signaling and other local factors. Several tumors in the pediatric population have features that resemble this more primitive “embryonal” cell. These tumors can be very undifferentiated or they can contain certain features that place them into a more specific category depending on cytoarchitecture or immunohistochemical staining. Included in this group are tumors such as medulloblastomas, primitive neuroectodermal tumors (PNET), and atypical teratoid/rhabdoid tumors (ATRT).
Germ Cell Tumors
Germ cell tumors are another group of tumors requiring special note. As with embryonic tumors, germ cell tumors arise from cells that are not commonly found in the adult brain. These tumors originate from cells in the developing embryo’s yolk sac endoderm that migrate throughout the embryo. They frequently are found in the pineal and suprasellar/pituitary region, as well as the third ventricle and posterior fossa. Germinomas are the most common germ cell tumors in the pediatric population.
Classification of Brainstem Gliomas
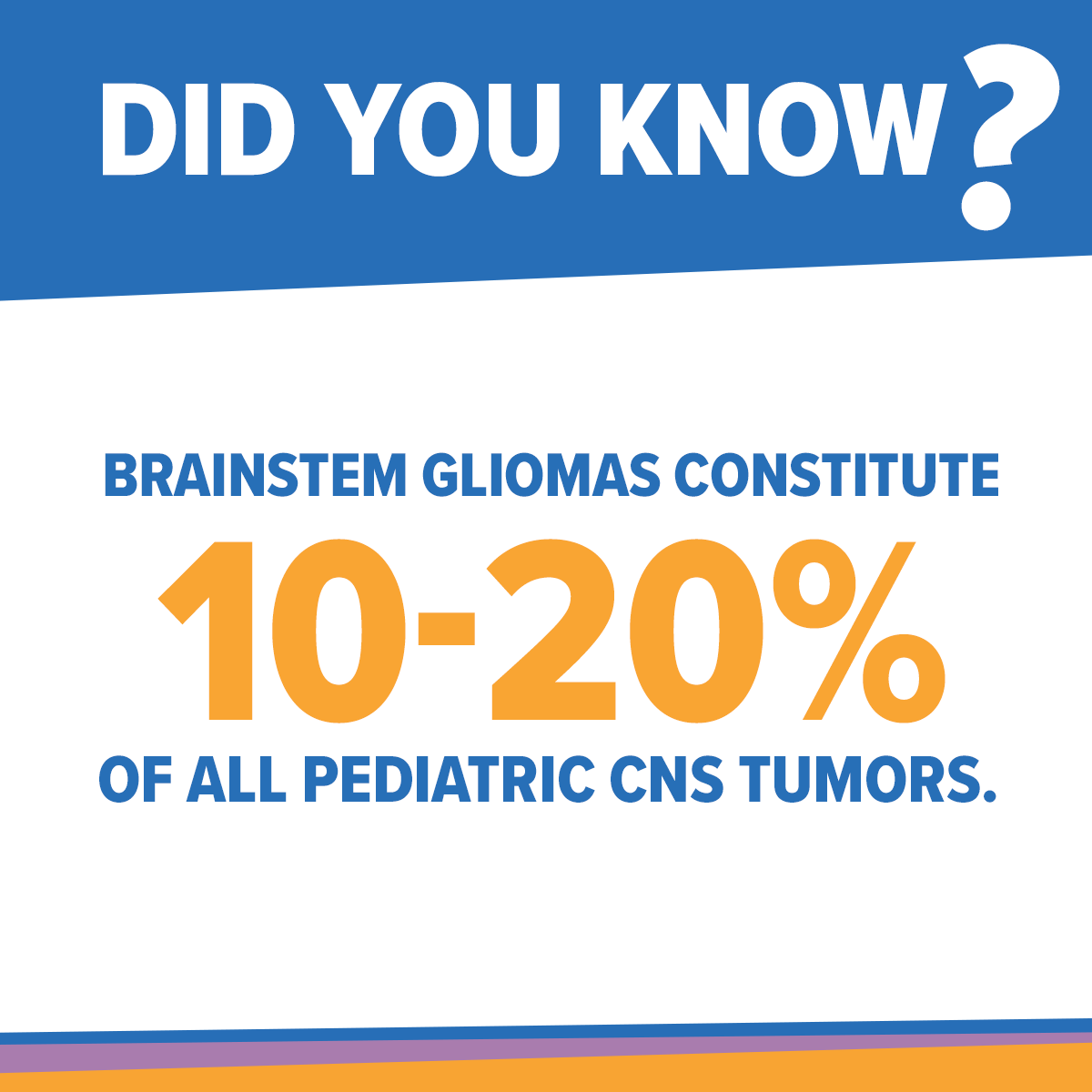
Overall, the most common brain tumors found in the pediatric population are pilocytic astrocytomas, malignant gliomas, and medulloblastomas. Within the glioma category, brainstem gliomas constitute 10–20% of all pediatric CNS tumors. We will narrow the scope of our discussion to brainstem gliomas, as they tend to present a unique and challenging tumor with its own classification scheme that provides a framework to predict growth patterns, surgical resectability, and overall prognosis.
Many classification schemes have been devised to categorize brainstem tumors based on imaging and tumor characteristics. All of these systems categorize tumors based on diffuse or focal imaging characteristics. Several more complex classification systems further divide the tumors based on location, growth pattern, and presence of hydrocephalus or hemorrhage.
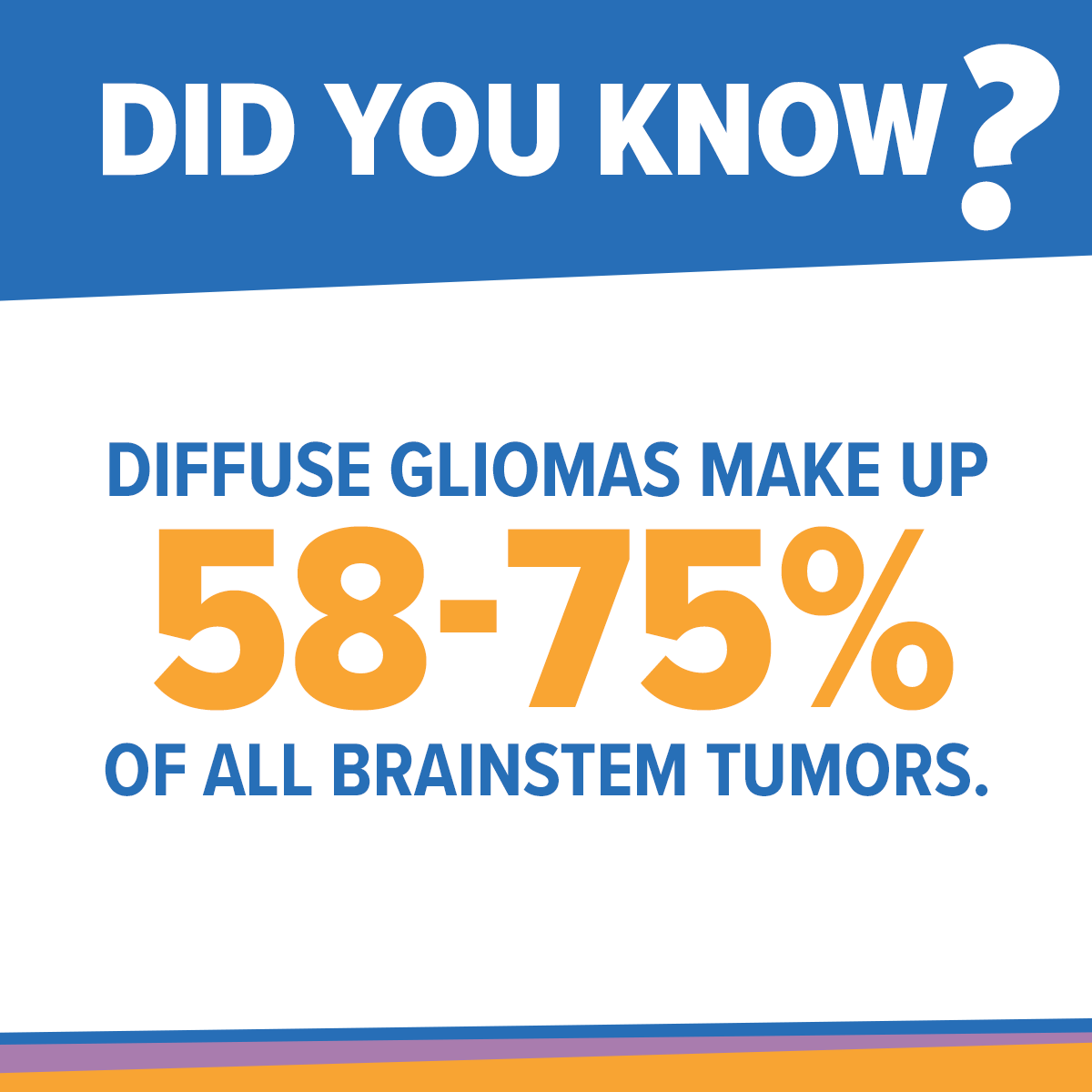
One of the main characteristics determined on imaging is the degree of focality; in other words, is the tumor diffuse and infiltrating or does it have a clearer demarcation of margin? Diffuse gliomas make up 58–75% of all brainstem tumors and are the most common tumor found in this location. On MRI imaging they have indistinct margins and are characterized by diffuse infiltration and swelling of the brainstem. These tumors are usually located within the pons, however they may also extend into other areas of the brainstem. These tumors have variable contrast enhancement and tend to be high-grade lesions. The usual histopathology is typically a malignant fibrillary astrocytoma, WHO grade III or IV.
Focal tumors have more clearly defined margins and, when in the brainstem, are usually found in the midbrain, pons, or medulla. They usually are not infiltrating and are not associated with swelling of adjacent structures, also known as edema. These focal tumors are often benign on histology and graded as WHO grade I or II, although cases of more aggressive tumors have been reported.
In addition to degree of focality, some classification schemes also consider whether the tumor is primarily inside the brainstem, which is defined as intrinsic, or if it resides mostly outside the brainstem, which is defined as exophytic. Exophytic brainstem gliomas arise from the subependymal glial tissue and the majority of the tumor is located in the fourth ventricle. These are usually well-defined tumors that are almost always low-grade gliomas.
Location of brainstem tumors is also a consideration when classifying them.For example, cervicomedullary tumors, found where the lower part of the brainstem connects to the top of the cervical spinal cord, tend to be slow growing and focal lesions and thus are considered benign low-grade astrocytomas. However, more aggressive cervicomedullary tumors, which are more infiltrative and grow up into the brainstem, have been found in this location.
Using these classification schemes—combining degree of focality (i.e. diffuse or well delineated), intrinsic or exophytic, and tumor location—health care providers can formulate a differential diagnosis and establish a reasonable treatment plan. Characteristics that may help further classify the tumor include direction and extent of tumor growth, degree of brainstem enlargement, hemorrhage or necrosis, and evidence of hydrocephalus.
Another simpler classification scheme divides brainstem tumors into typical and atypical brainstem gliomas. The term typical brainstem gliomas is synonymous with the term diffuse intrinsic pontine gliomas (DIPG). As mentioned earlier, these tumors are diffuse and infiltrative, located in the pons but potentially extending into other areas of the brainstem. Surgery or biopsy of these lesions is not usually recommended at this time, unless the diagnosis is in question. Atypical gliomas include the focal lesions which are well circumscribed. They may be contained in the brainstem or may grow out in cysts or outside of the brainstem. Unlike typical brainstem gliomas, the atypical gliomas tend to arise from the midbrain (the top of the brainstem) or the medulla. These atypical tumors tend to be lower grade lesions which may be amenable to some degree of surgical resection or biopsy.
The majority of brainstem tumors are diffuse pontine gliomas that are mainly high grade on histological examination and have poor prognosis. DIPG.org covers the current treatment strategies, role for surgery, radiation and chemotherapy, and future directions in the treatment of DIPG.
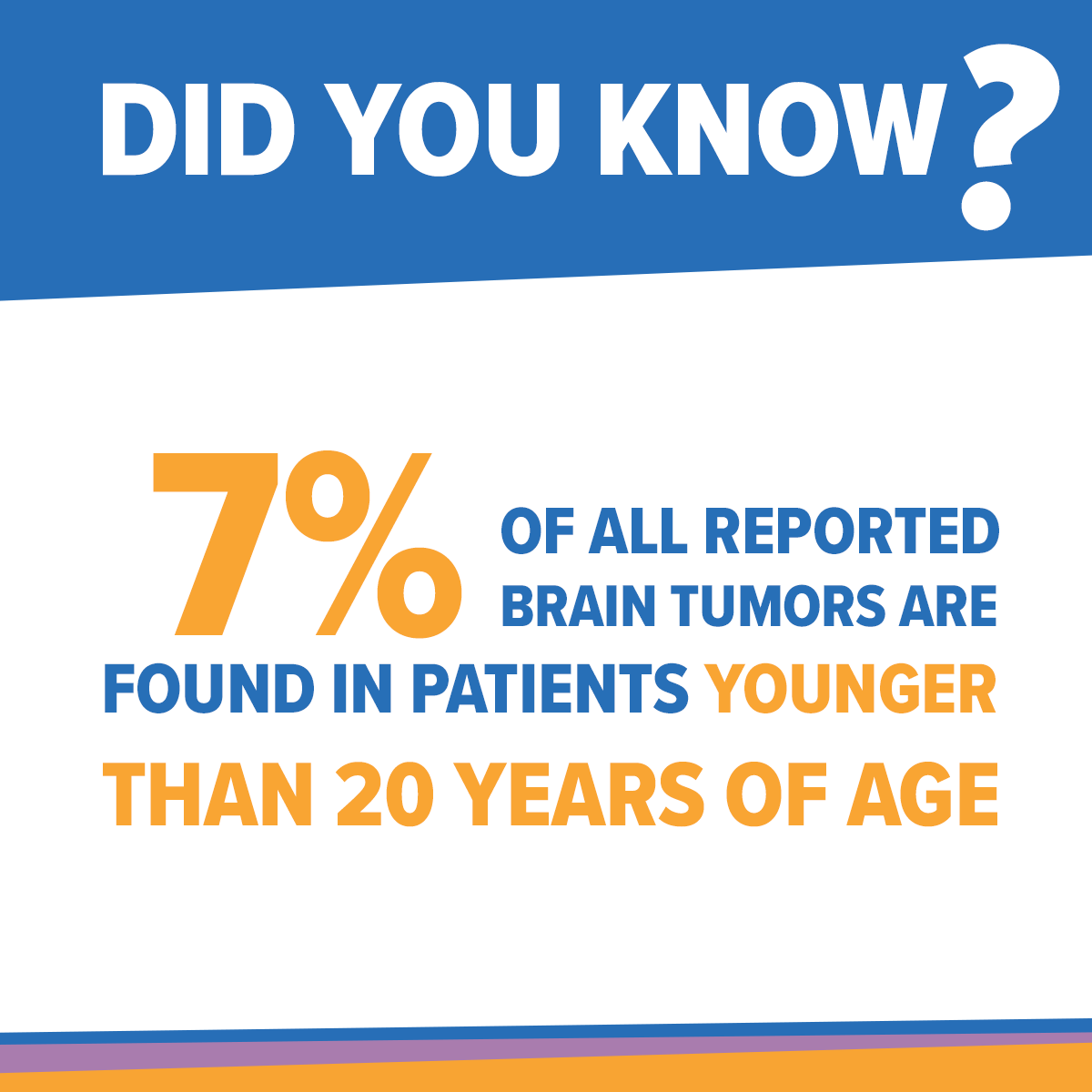
Cancer in Children
Brain tumors are the leading cause of cancer death in the pediatric population. They are the second most common malignancy in children behind leukemia, and the most common solid tumor found in the pediatric population. According to the 2009 statistical report of the Central Brain Tumor Registry of the United States, 7% of all reported brain tumors are found in patients younger than 20 years of age. The overall incidence of brain tumors found in the age group comprising 0–19 year olds is 4.58 per 100,000 individuals. Overall, there is a slight male predominance in pediatric brain tumors, however, depending on the individual histology, certain tumor subtypes are found more frequently in females. Brain tumors are also more common in whites than blacks. The age distribution varies depending upon the specific tumor, with certain tumors such as pilocytic astrocytomas, malignant gliomas, and medulloblastomas more common in the younger pediatric population of 0–14 year olds, while germ cell tumors are more common in 15–19 year old age group.
The majority of pediatric tumors are located in the cerebral hemispheres, mainly within the frontal, parietal, temporal, or occipital lobes, overall making up 24% of brain tumors. 16% of tumors are found in the cerebellum, 12% in the brainstem, 6% within the ventricles, 11.6% in the pituitary, and 3.2% in the pineal region. The remaining less common sites include the meninges, the cranial nerves, the spinal cord, and other brain areas.
Content used with permission from the American Childhood Cancer Organization. Hoffman, Ruth, editor. Understanding The Journey: A Parent’s Guide to DIPG. American Childhood Cancer Organization, 2012. Print.
Contributing Authors:
- Violette Renard Recinos, MD
- George I. Jallo, MD

